Sohar Health
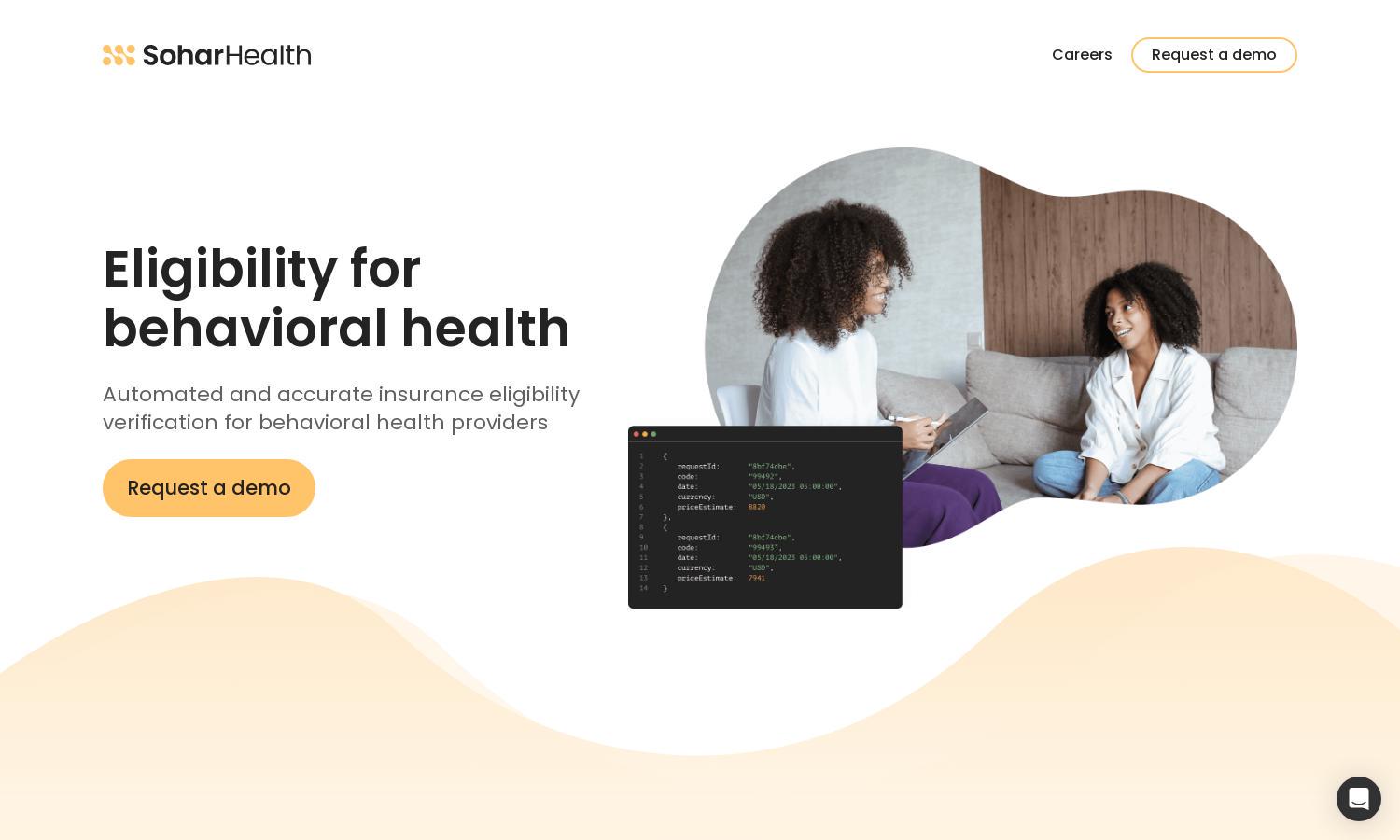
About Sohar Health
Sohar Health is designed for behavioral health companies aiming for efficiency in patient eligibility verification. Through powerful APIs, it offers automated and accurate insurance checks, significantly reducing claims denials and enhancing patient intake. The platform empowers users to deliver exceptional care while optimizing operational resources.
Sohar Health offers flexible pricing plans to accommodate various organizational sizes. Each subscription tier provides access to vital eligibility verification tools. Upgrading unlocks additional features tailored for enhanced accuracy and operational efficiency, enabling users to maximize revenue while minimizing claim denials.
Sohar Health boasts a user-friendly interface designed for intuitiveness and seamless navigation. The layout ensures quick access to vital features, including detailed insurance verification. Users benefit from interactive elements that enhance their experience, making eligibility checks efficient and straightforward.
How Sohar Health works
Users begin their journey with Sohar Health by creating an account and integrating their systems via powerful APIs. Once onboard, they can easily navigate the dashboard to input patient data for eligibility verification. The platform automates insurance checks, providing detailed results that enhance patient intake and reduce claims denials. Sohar Health prioritizes usability, ensuring that even non-technical staff can efficiently access and utilize core features.
Key Features for Sohar Health
Automated Patient Eligibility Verification
Sohar Health features automated patient eligibility verification, allowing behavioral health companies to efficiently check insurance coverage. This unique function provides precise eligibility data, enhancing patient intake and significantly reducing claim denials, ultimately driving revenue growth for providers.
Insurance Discovery
Sohar Health offers comprehensive insurance discovery, simplifying the process of determining patient coverage. By leveraging advanced technology, this feature equips behavioral health providers with accurate coverage insights, allowing them to deliver better patient care while minimizing operational risks.
Developer-Friendly APIs
Sohar Health's developer-friendly APIs facilitate seamless integration, empowering healthcare providers to enhance operational efficiency. This distinctive feature ensures rapid deployment and allows users to customize their eligibility verification processes, driving improved outcomes in behavioral health services.
You may also like: